The Pediatric Neurotrauma Lab, directed by Andrew Reisner, MD, is a multi-institutional collaboration between Children’s Healthcare of Atlanta and Emory University. Our mission is to establish a basic science research program focused on pediatric traumatic brain injury (TBI). We work to improve the health and quality of life of children living with acute neurological injuries, specifically TBI.
Through our large volume of pediatric neurotrauma patients, we use translational research to improve patient care. We collaborate with local and national researchers of all disciplines to advance the understanding and treatment of TBI.
The Pediatric Neurotrauma Lab’s mission is to facilitate research that can improve the treatment and outcomes of traumatic brain injuries in children.
Areas of Study include:
- Concussions
- Traumatic Brain Injury
- Biomarkers from acquired Brain Injury
- Firearm Injuries
- Health Disparities & Social Determinants of Health
Andrew Reisner, MD, FACS, FAAP, Pediatric Neurosurgery
Director and Principal Investigator
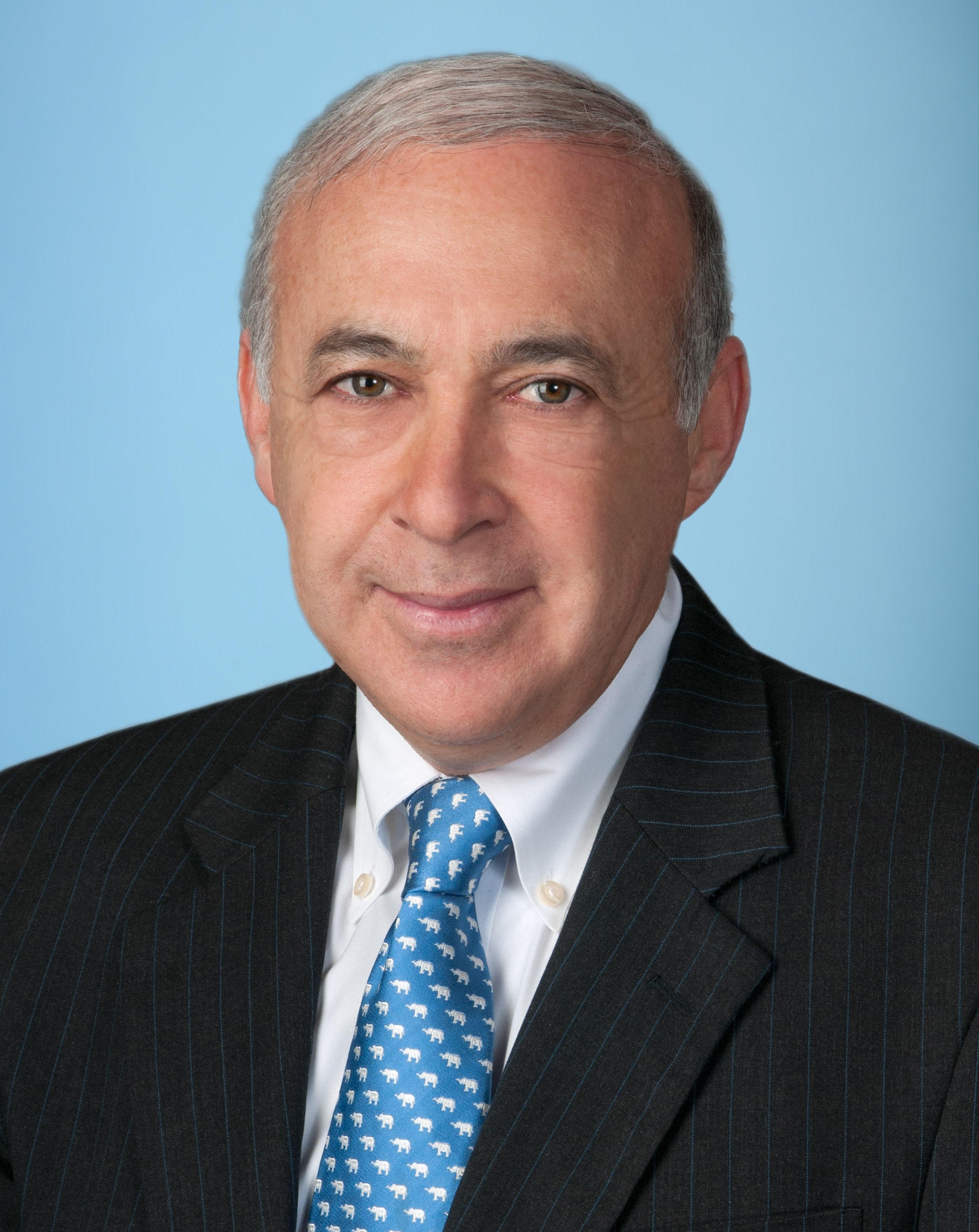
Professor Andrew Reisner is a pediatric neurosurgeon. He completed his neurosurgery residency at Emory University and a pediatric neurosurgery fellowship at the University of California, San Francisco. He has been an attending neurosurgeon at Children’s Healthcare of Atlanta (CHOA) for almost 30 years. He has a large clinical practice and has averaged over 400 surgical cases annually over this period.
Dr. Reisner’s research activity has focused on neurotrauma. He established the severe TBI and concussion clinical programs at CHOA as well as the translational research-focused Pediatric Neurotrauma Lab. He has authored over 150 papers, abstracts and book chapters and given over 300 presentations nationally and internationally.
Dr Reisner was appointed Elaine and John C. Carlos Chair of Neurotrauma at Children’s Healthcare of Atlanta and was awarded the Children’s Care Network "Award of Merit" for significant contributions to Pediatrics. He is currently Chair, Neurotraumatology, of the World Federation of Neurosurgical Societies (WFNS).
Laura Blackwell, PhD, Pediatric Neuropsychology
Principal Investigator

Laura Blackwell, PhD, ABPP-CN, is a Pediatric Neuropsychologist and Co-Director of the Pediatric Neuropsychology Fellowship Program at Children’s Healthcare of Atlanta and serves as Associate Professor at Emory University School of Medicine. Dr. Blackwell primarily cares for children and adolescents following an acquired brain injury, including moderate and severe head injuries, concussion, and stroke. She joined Children’s and Emory in 2016 following her fellowship training in clinical neuropsychology at Boston Children's Hospital. Prior to her fellowship, she completed her doctoral degree at the University of Miami followed by a predoctoral internship at Kennedy Krieger Institute/Johns Hopkins School of Medicine, with primary rotations in neuropsychology and pediatric psychology.
As a principal investigator in the Pediatric Neurotrauma Lab, her research focuses on examining different types of biological biomarkers that could help provide information about management and predictors of outcomes in pediatric traumatic brain injury. Dr. Blackwell and her team want to better understand how aspects of a child’s biological system as well as their premorbid psychological, behavioral, and environmental history, influence their recovery after an injury. She focuses on different acute and chronic markers of injury, including an interest in an inflammatory marker called osteopontin. Dr. Blackwell also leads the lab’s research on social determinants of health and manages students and their projects.
Meena Verma, MD
Research Team Lead

Meena is a pediatrician and clinical researcher with 20+ years of clinical experience with subject matter expertise in design-execution of clinical research studies. A public health professional and passionate servant leader who led an acclaimed 501(c)(3) non-profit. As an Executive Director and Chief Mentor, she led extensive domestic and global public health work. Meena is currently the Neurosciences Research Team Lead at the Scottish Rite Campus. She oversees studies under several Neurology disciplines, such as Neuroimmunology, Neurosurgery, Craniofacial, and Urology.
Jacob R. Lepard, MD, Pediatric Neurosurgery
Co-Investigator

Jacob Lepard was born in the southeastern USA. He completed neurosurgical training at the University of Alabama at Birmingham, during which time he participated in Paul Farmer Global Surgery Fellowship at the Harvard Program in Global Surgery and Social Change. He then went on to complete post-graduate fellowships in complex spine surgery at the UAB Department of Orthopedics and Pediatric Neurosurgery at Texas Children’s Hospital/Baylor College of Medicine. He now practices at Children’s Healthcare of Atlanta/Emory University School of Medicine. His areas of focus include neurotrauma, hydrocephalus and spina bifida, cerebral palsy and spasticity, fetal neurosurgery, and global neurosurgical capacity building and education.
Mahwish Javed, MS, MPH
Program Manager, Neurotrauma

Mahwish joined Children’s in 2016. She is Program Manager in Neurosciences. Her primary focus is to provide effective leadership and overall management of 4 outpatient large complex, multidisciplinary clinics. This entails, overseeing all clinical and non-clinical operations including, tracking progress toward clinical goals, facilitate coordination among participating partners, evaluate clinical data, and coordinate submission of new project proposals, preparation of manuscripts and report project status to leadership. She is also responsible for strategic planning, program design/implementation, marketing, and Identifying new funding opportunities.
Mahwish is Pakistani American and was born and raised in Pakistan. She obtained her Master of Public Health in Public Health Informatics from University of Illinois – Chicago, Illinois, and Masters of Science in Health Communications from University of Peshawar – Pakistan. In her free time Mahwish enjoys travelling and spending time with her husband and two boys (ages 16 and 17).
Anna Trofimova, MD, PhD, Pediatric Neuroradiology

Dr. Trofimova is an assistant professor of radiology and imaging sciences and a pediatric neuroradiologist at Children's Healthcare of Atlanta. Her research focus is on investigating the role of advanced diagnostic techniques in assessment of microstructural and functional brain changes in health and disease. She is a recipient of RSNA Research Resident and RSNA Research Fellow grants for investigating functional brain connectivity changes underlying vestibular symptoms persistence after mild traumatic brain injury. Dt. Trofimova earned her medical degree from Saint Petersburg State Medical University and a PhD from S.M. Kirov Medical Military Academy, both in Russia. She completed diagnostic radiology residency as well as a fellowship in neuroradiology and a fellowship in pediatric neuroradiology at Emory University School of Medicine and is board certified in both diagnostic radiology and neuroradiology.
Makda Mulugeta, BS
Research Coordinator

Makda Mulugeta is a Research Coordinator at the Pediatric Neurotrauma Lab and recent graduate of Emory University. She works on TBI studies and recently presented at the 2023 Congress of Neurological Surgeons Annual Meeting, where she won Top 3 Disparities in Health Poster Award. She is passionate about improving global health, mitigating health disparities, and the intersection of medicine and anthropology. In her spare time, she volunteers with Children's Healthcare of Atlanta's Injury Prevention Program to prevent traumatic injuries in local communities.
Gabrielle Bailey, MPH
Research Assistant

Gabrielle Bailey serves as a Research Assistant for the Pediatric Neurotrauma Lab. She holds her bachelor’s degree in Human Health from Emory University with an emphasis on public health research development and both the biological and sociological aspects of health practice. Gabrielle currently works on TBI studies and recently graduated with her MPH from Emory.
Sarah Maddox, BA
Research Coordinator

Sarah graduated from Millsaps College with a B.A. in psychology and a minor in anthropology. Her research interests include neurocognitive profiles of pediatric epilepsy patients, social and adaptive functioning for post-TBI patients, and comparison of pre-surgical and post-surgical neuropsychological testing. She has worked with PNL since 2022 and assists Dr. Blackwell in her neuropsychological research outside of PNL as well. Sarah is currently a neurosciences research coordinator focusing on neuropsychology and neurology.
PNL Collaborators
Kevin Wang, PhD, Director of the Center for Neurotrauma, MultiOmics & Biomarkers (CNMB), Professor & Vice-Chair of Neurobiology and Faculty of the Neuroscience Institute at Morehouse School of Medicine.

Firas H. Kobaissy, PhD, Associate Director of the Center for Neurotrauma, MultiOmics & Biomarkers (CNMB), Professor of Neurobiology and Faculty of the Neuroscience Institute at Morehouse School of Medicine.

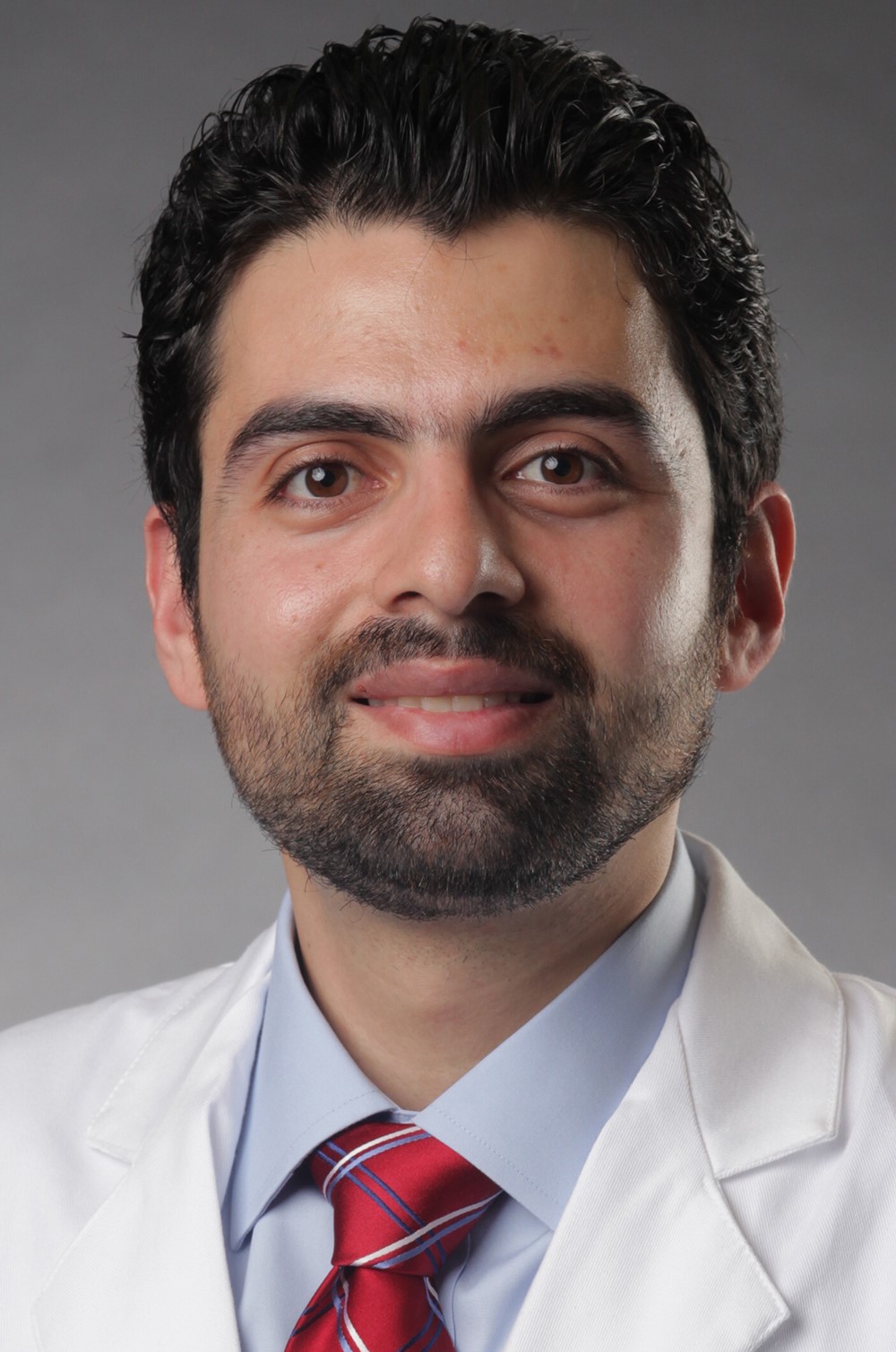
Ali Alawieh, MD, PhD, PGY-5 at the Department of Neurosurgery, Emory University School of Medicine.
Current PNL Students
Kendall Parsons
Leslie Avellaneda

Joshitha Arora
Alvin Onyewuenyi, MPH

Former Students:
Keri Kramer
Ana Shin
Hannah Myers, Medical College of Georgia
Andrew Appert, Case Western Reserve School of Medicine
Maggie Martinez
Annabelle Thomas
Megan Jungers
Eva de Valle Martinez, Texas Children's Hospital
Ruhika Aguru
Recent Publications:
- Parsons K, Mulugeta MG, Bailey G, Gillespie S, Johnson LM, Myers HE, Reisner A and Blackwell LS (2024) Association between social determinants of health and pediatric traumatic brain injury outcomes. Front. Neurol. 15:1339255. doi: 10.3389/fneur.2024.1339255
- Mulugeta MG, Bailey G, Parsons K, Gillespie S, Johnson LM, Doh KF, Reisner A and Blackwell LS (2024) Trends in pediatric firearm-related injuries and disparities in acute outcomes. Front. Public Health 12:1339394. doi: 10.3389/fpubh.2024.1339394
- Blackwell, L.S, Wali, B., Xiang, Y., Alawieh, A., Sayeed, I., Reisner, A. (2023) Prognostic value of plasma biomarkers S100B and osteopontin in pediatric TBI: A prospective analysis evaluating acute and 6-month outcomes after mild to severe TBI. Biomedicines, 11(8): 2167.
- Laura S. Blackwell, Robert Grell. Pediatric Traumatic Brain Injury: Impact on the Developing Brain, Pediatric Neurology, Volume 148, (2023), Pages 215-222, ISSN 0887-8994, https://doi.org/10.1016/j.pediatrneurol.2023.06.019.
- Reisner, A., Blackwell, L. S., Sayeed, I., Myers, H. E., Wali, B., Heilman, S., ... & Rostad, C. A. (2022). Osteopontin as a biomarker for COVID-19 severity and multisystem inflammatory syndrome in children: A pilot study. Experimental Biology and Medicine, 247(2), 145-151.
- Watson, W. D., Suskauer, S. J., Askin, G., Nowak, S., Baum, K. T., Gerber, L. M., ... & Shah, S. A. (2021). Cognitive recovery during inpatient rehabilitation following pediatric traumatic brain injury: a pediatric brain injury consortium study. Journal of head trauma rehabilitation, 36(4), 253-263.
- Gao, N., Zhang-Brotzge, X., Wali, B., Sayeed, I., Chern, J. J., Blackwell, L. S., ... & Reisner, A. (2020). Plasma osteopontin may predict neuroinflammation and the severity of pediatric traumatic brain injury. Journal of Cerebral Blood Flow & Metabolism, 40(1), 35-43.
- Blackwell, L.S., Martinez, M., Fournier-Goodnight, A., Figueroa, J., Appert, A., Vats, A., Wali, B., Sayeed, I., & Reisner, A. (2020). Patterns of osteopontin expression in abusive head trauma compared with other causes of pediatric traumatic brain injury. Journal of Pediatrics, 227: 170-175.
- Reisner, A., Ralston, A. K., Vats, A., Sawvel, M. S., & Blackwell, L. S. (2019). Commentary: guidelines for the management of pediatric severe traumatic brain injury: update of the brain trauma foundation guidelines, executive summary. Neurosurgery, 85(2), E384-E385.
- Murdaugh, D. L., King, T. Z., Sun, B., Jones, R. A., Ono, K. E., Reisner, A., & Burns, T. G. (2018). Longitudinal changes in resting state connectivity and white matter integrity in adolescents with sports-related Concussion–Erratum. Journal of the International Neuropsychological Society, 24(8), 890-890.
- Reisner, A., Chern, J. J., Walson, K., Tillman, N., Petrillo-Albarano, T., Sribnick, E. A., ... & Vats, A. (2018). Introduction of severe traumatic brain injury care protocol is associated with reduction in mortality for pediatric patients: a case study of Children’s Healthcare of Atlanta’s neurotrauma program. Journal of Neurosurgery: Pediatrics, 22(2), 165-172.
Non-neurotrauma related
- Ilardi, D., Alexander, N., Xiang, Y., Figueroa, J., & Blackwell, L. (2022). Social-environmental factors as mediators of IQ and achievement differences across race groups in adolescents with high risk congenital heart disease. Child Neuropsychology, 1-18.
- Kashyap, N., Morris, M., Loerinc, L. B., Benoit, M., Blackwell, L., Howarth, R., & Gombolay, G. (2022). The neutrophil-to-lymphocyte ratio is associated with intubation in pediatric anti-NMDA receptor encephalitis: A retrospective study. Journal of Neuroimmunology, 370, 577931.
The following list is student presentations. For recent PNL investigator presentations, check out our News & Updates tab!
Student Presentations:
2023 Congress of Neurological Surgeons
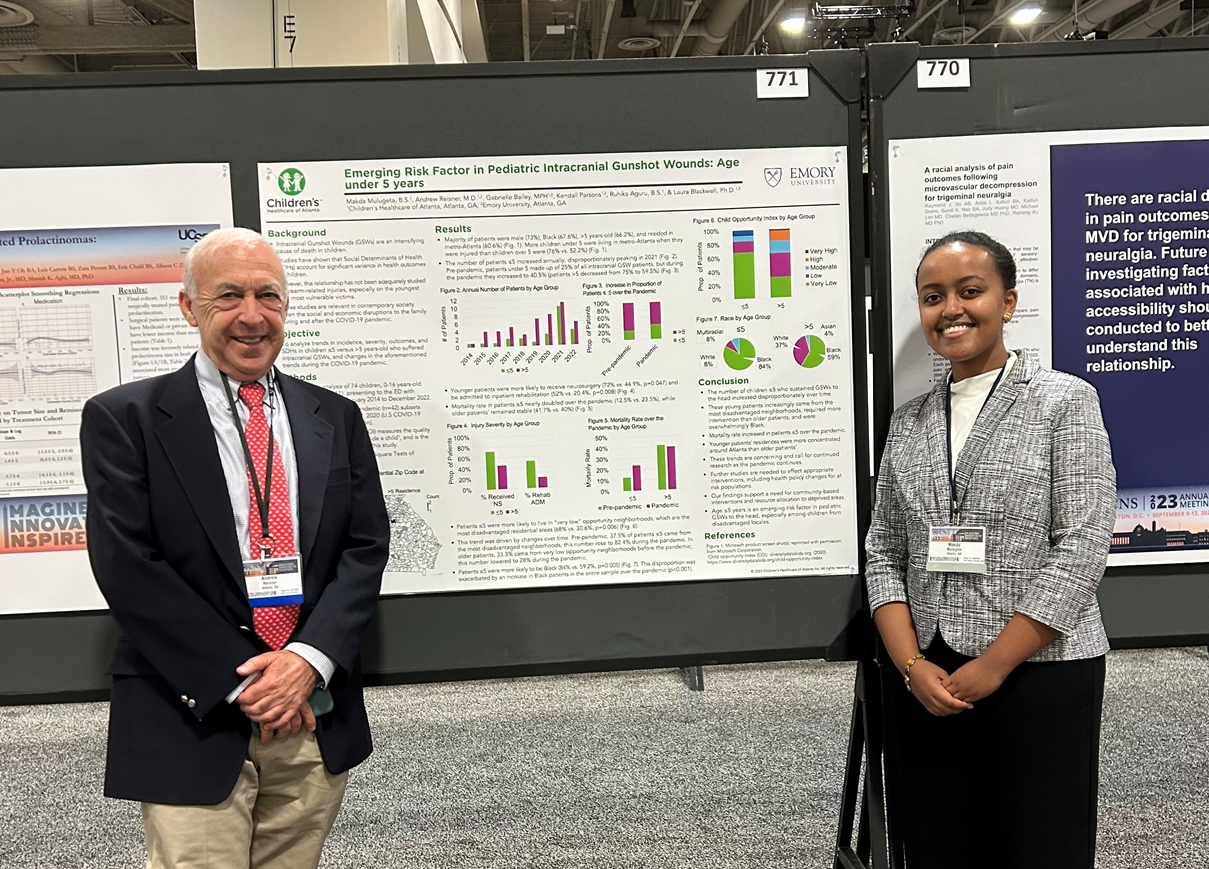
- Makda Mulugeta "Emerging Risk Factor in Pediatric Intracranial Gunshot Wounds: Age under 5 years” *Top 3 Disparities in Healthcare Poster
2023 National Neurotrauma Society (Abstracts Published)
-
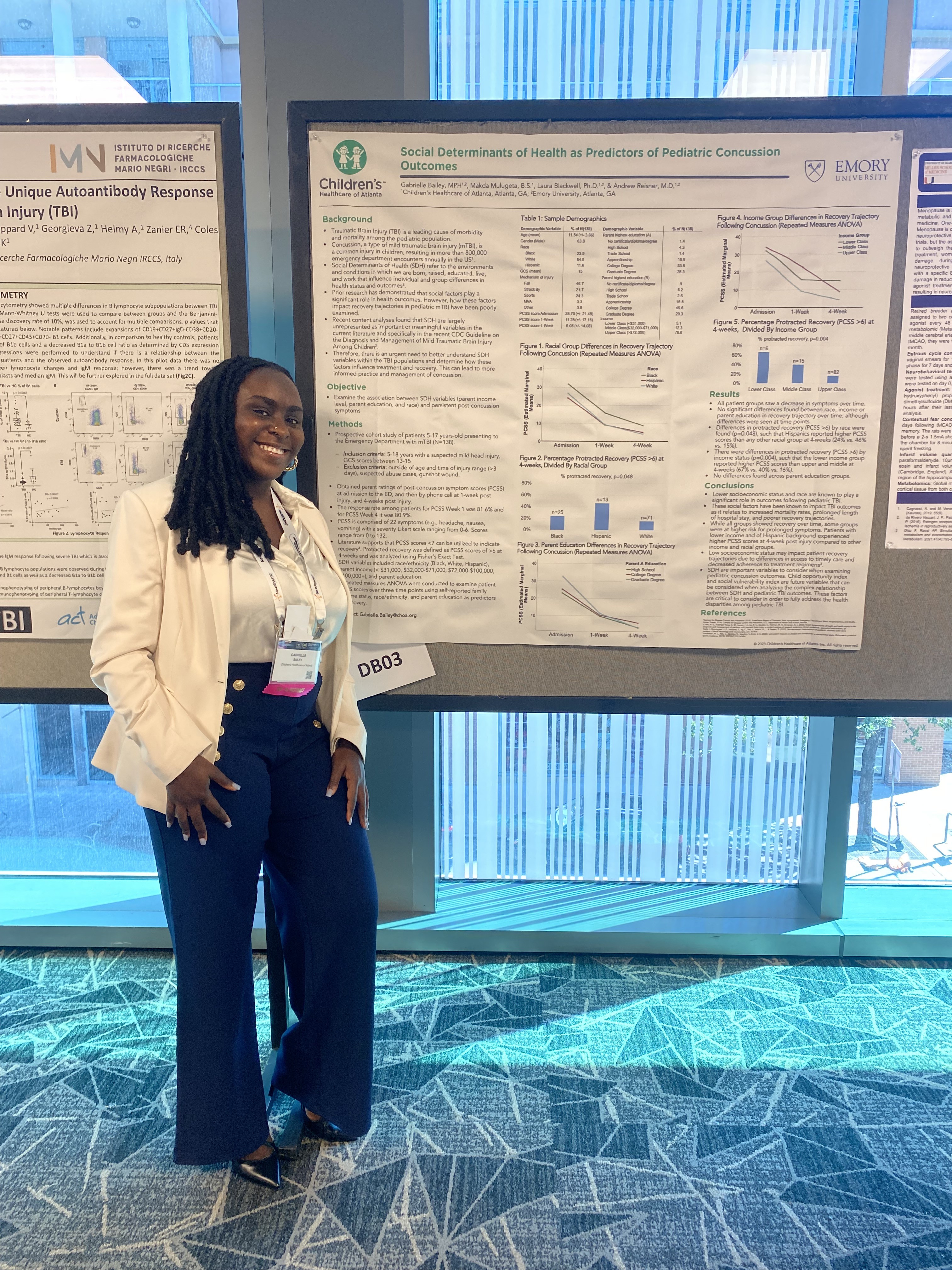
Gabrielle Bailey "Social Determinants of Health as Predictors of Pediatric Concussion Outcomes” (oral presentation) *Top 20 Trainee Abstracts, Trainee Diversity Award
-
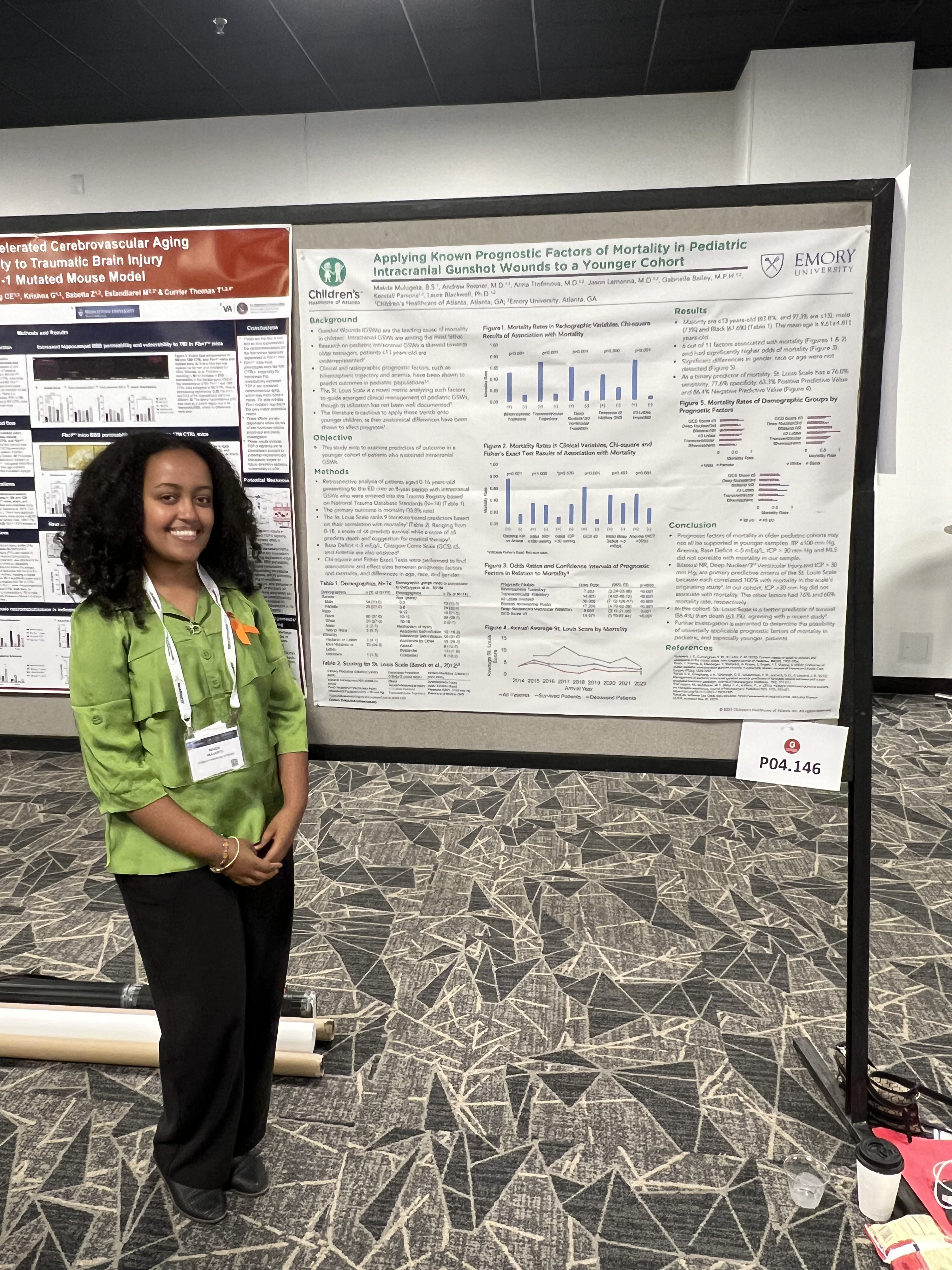
Makda Mulugeta “Applying Known Prognostic Factors of Mortality in Pediatric Intracranial Gunshot Wounds to a Younger Cohort"
-
Kendall Parsons “Socioeconomic Health Disparities in Pediatric Traumatic Brain Injury: Comparisons of Hispanic and Non-Hispanic Children”
2023 Southeastern Pediatric Research Alliance Conference
- Ruhika Aguru “The Relationship between Child Opportunity Index and Mortality in Pediatric Patients with Intracranial Firearm Injuries” (oral presentation)
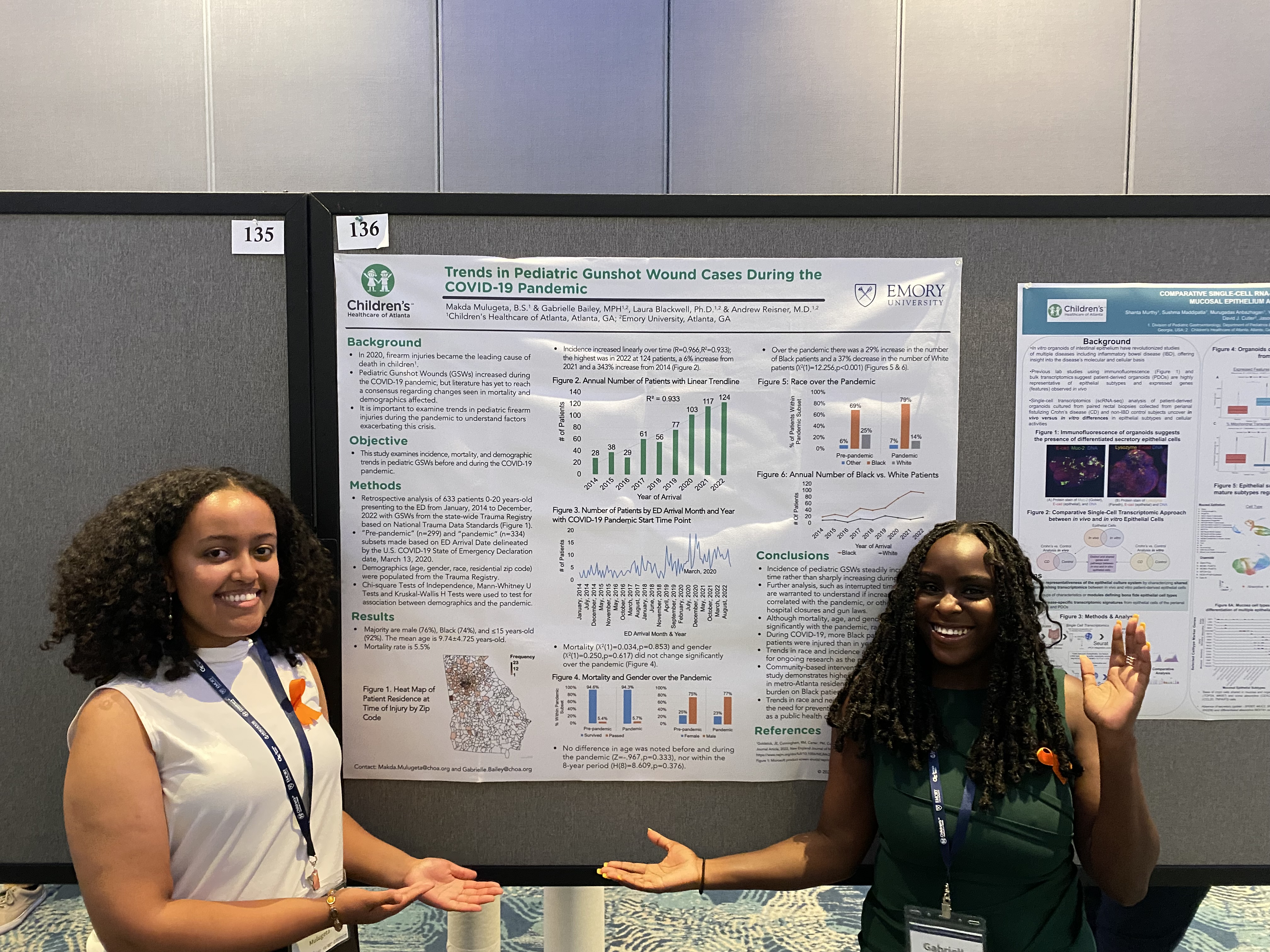
- Makda Mulugeta & Gabrielle Bailey “Trends in Pediatric Gunshot Cases During the COVID-19 Pandemic”
2022 National Neurotrauma Society (Abstracts Published)
- Andrew Appert “Increased levels of osteopontin in children with subdural hematomas due to abusive head trauma”
- Makda Mulugeta “Implications of Race and Socioeconomic Status on Pediatric Traumatic Brain Injury Severity and Outcome” *Trainee Diversity Award
2022 Southeastern Pediatric Research Alliance Conference
- Andrew Appert “Increased levels of osteopontin in children with subdural hematomas due to abusive head trauma”
-
Eva del Valle Martinez “Follow-up visit attendance in children following a traumatic brain injury”
-
Keri Kramer “Neuropsychiatric outcomes in children with traumatic brain injuries”
-
Makda Mulugeta “Implications of Race and Socioeconomic Status on Pediatric Traumatic Brain Injury Severity and Outcome”
-
Hannah Myers “Comparing plasma biomarker profiles in complicated versus uncomplicated mild TBI in children”
- Anabelle Thomas “Gender and age differences in recovery trajectories following pediatric concussion”
Recent Grants:
- Elaine and John C. Carlos Endowed Chair of Neurotrauma, $2 million
- Children’s Healthcare of Atlanta and Emory University, Established 2017
- National Institutes of Health R21 grant, $466,650
- Reisner A., Sayeed I. - PI; Blackwell L.S.-Co-I; - Osteopontin as a Blood Biomarker in Severe Pediatric Brain Injury.
- Funded March 1, 2018- February 29, 2022
- Emerging Leaders for Children’s group, Estimated at $250K
- Concussion Program as beneficiary of their 2017 fundraising efforts, Funded 2017
- Andrew Reisner Traumatic Brain Injury Fund, Total Donations > $500,000
- Established by patients/families
- CHOA Board of Trustees Pediatric Neurotrauma Lab, $500,000
- Reisner A., Blackwell L.S., Sayeed, I. – PI , Funded 2018-2021
- Children’s Healthcare of Atlanta Concussion Program, $250,000
- Variety of Private and Corporate Donors
- 1 UO1 CE002939-01 Grant, $5 million
- Gioia, G.A., Ratcliff, J., Simon, H.K.- PI – Promoting Recovery in Children Who Sustain a Mild Traumatic Brain Injury: The TBI Evaluation and Management (TEaM) Toolkit, Funded 2018
For a comprehensive list of PNL's abstracts, peer reviewed publications, grants, and presentations, email us here!
March 2024:
Dr. Reisner attended the 2024 International Conference on Recent Advances in Neurotraumatology in Jaipur, India! As the Chairman of the Neurotrauma Committee at the World Federation of Neurological Surgeons, he helped organize this successful event!

The theme this year was Stimulating Innovations in Neurotrauma, and the conference was well covered by local media!

In line with the theme, Dr. Reisner presented on post-traumatic aneurysms and the value of osteopontin as a biomarker.

In addition, he served as a delegate for a discussion about neurotrauma and road safety in India, which was followed by a walkathon for safer roads.

December 2023:
Dr. Blackwell is this month's Emory School of Medicine Research Spotlight!
She spoke about her research at PNL and why she's compelled to study TBIs:
“I have seen two patients with very similar traumatic brain injuries, but one patient discharged from the hospital in a disorder of consciousness while the other discharged and was walking, talking, and able to go back to school and home. We have a poor understanding of why kids’ outcomes are so discrepant. So for me, it is important to learn how and why these kids have very different trajectories. We want to be better at understanding outcomes so that it can lead to improved management.”
Read her spotlight article here!
Also in December, Dr. Reisner, Dr. Blackwell, Dr. Lepard and PNL Collaborators Dr. Wang and Dr. Alawieh attended the World Federation of Neurosurgical Society's 18th World Congress of Neurosurgery in Cape Town, South Africa!

PNL pictured with Dr. James Johnson from UAB Medicine.

Dr. Reisner pictured presenting on Traumatic Brain Injury Biomarkers in Children: Opportunities and Challenges, and chairing sessions in Neurotrauma and Masterclass in Research: Neurotrauma. Dr. Reisner served as the Chair of Neurotrauma for 2023 WFNS.

Dr. Blackwell pictured presenting on Utilizing Outcome Measures in Pediatric TBI and an abstract on Inflammation Disrupts Networks of Attention and Executive Function after Pediatric Traumatic Brain Injury: A Pilot Study.
Dr. Lepard pictured presenting on Incomplete Atlanta-Occipital Dissociation: Thoughts on Diagnosis and Management. He also presented an abstract on Hindbrain Herniation as a Criteria for Fetal Myelomeningocele Repair: A Natural History Study, and chaired a session on Innovating and Working with Industry: Neurotrauma.
PNL Collaborators Dr. Kevin Wang and Dr. Ali Alawieh were also in attendance and presented!
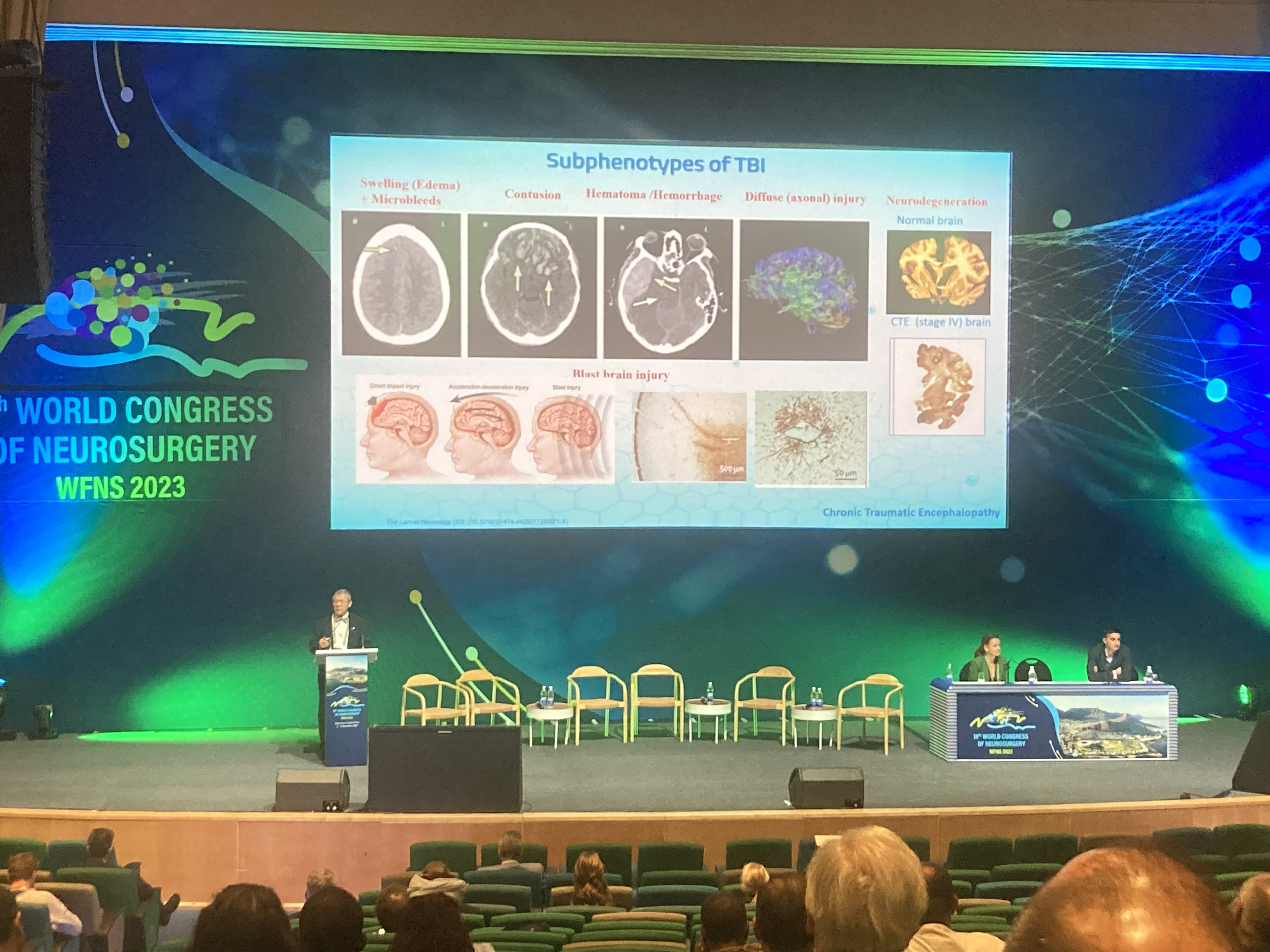
Dr. Wang pictured giving a plenary adress on How Blood-based Biomarker Tests can Reshape the way we Manage and Treat the Injured Brain. He also chaired sessions in Neurotrauma and Innovating and Working with Industry: Neurotrauma.
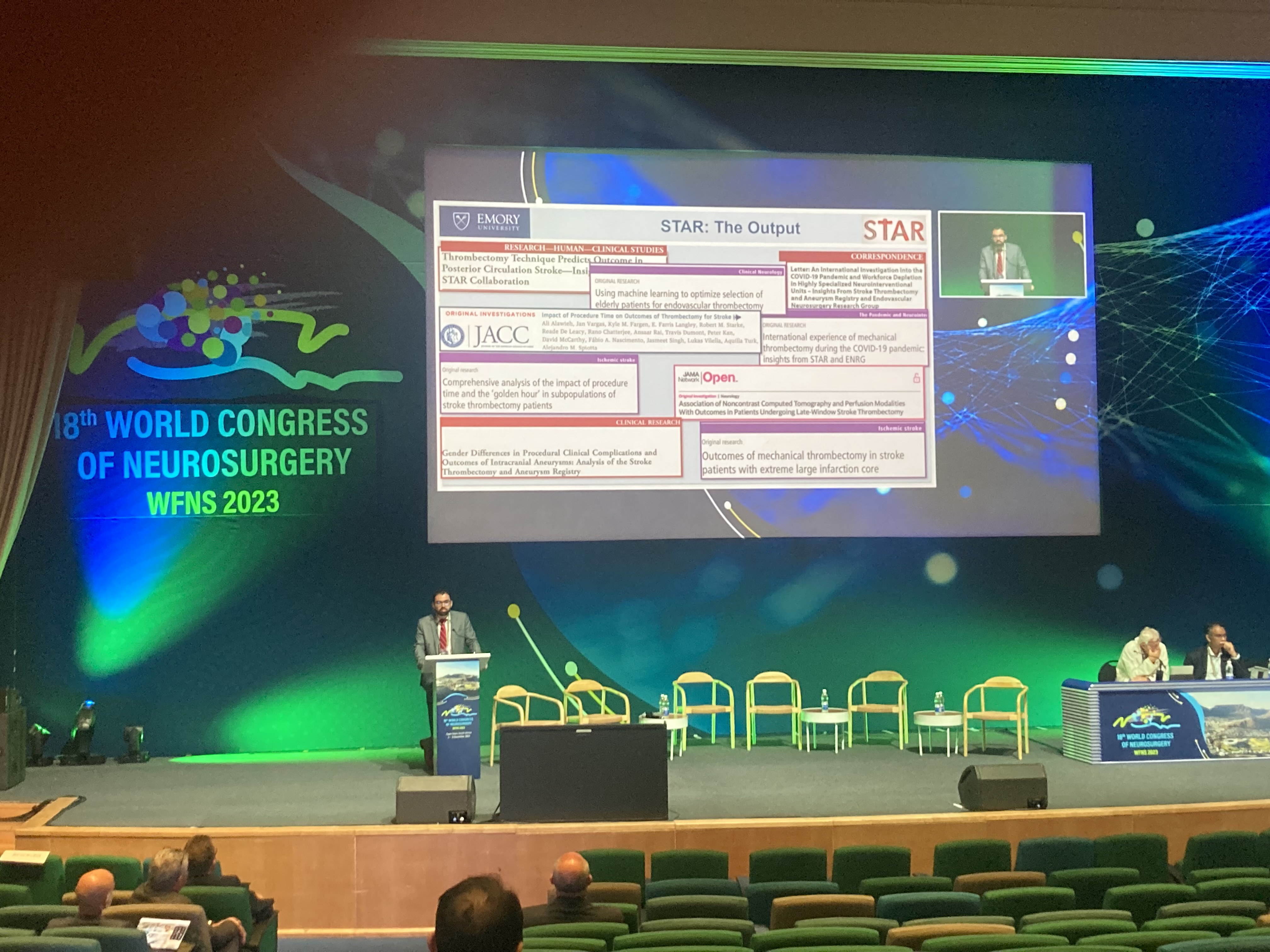
Dr. Alawieh pictured presenting on Dissecting the Role of Complement in Triggering Acute TBI and Its Progression to Chronic Encephalopathy. He also presented three abstracts: A Pooled Analysis of Management and Outcomes in Pediatric Infectious Intracranial Aneurysms, Site-specific Suppression of Complement C3 Activation Halts the Progression of Neuroinflammation after Traumatic Brain Injury – A Translational Approach, and The Stroke Thrombectomy and Aneurysm Registry (STAR) - An International Consortium for Advancing Management of Cerebrovascular Disease.
November 2023:
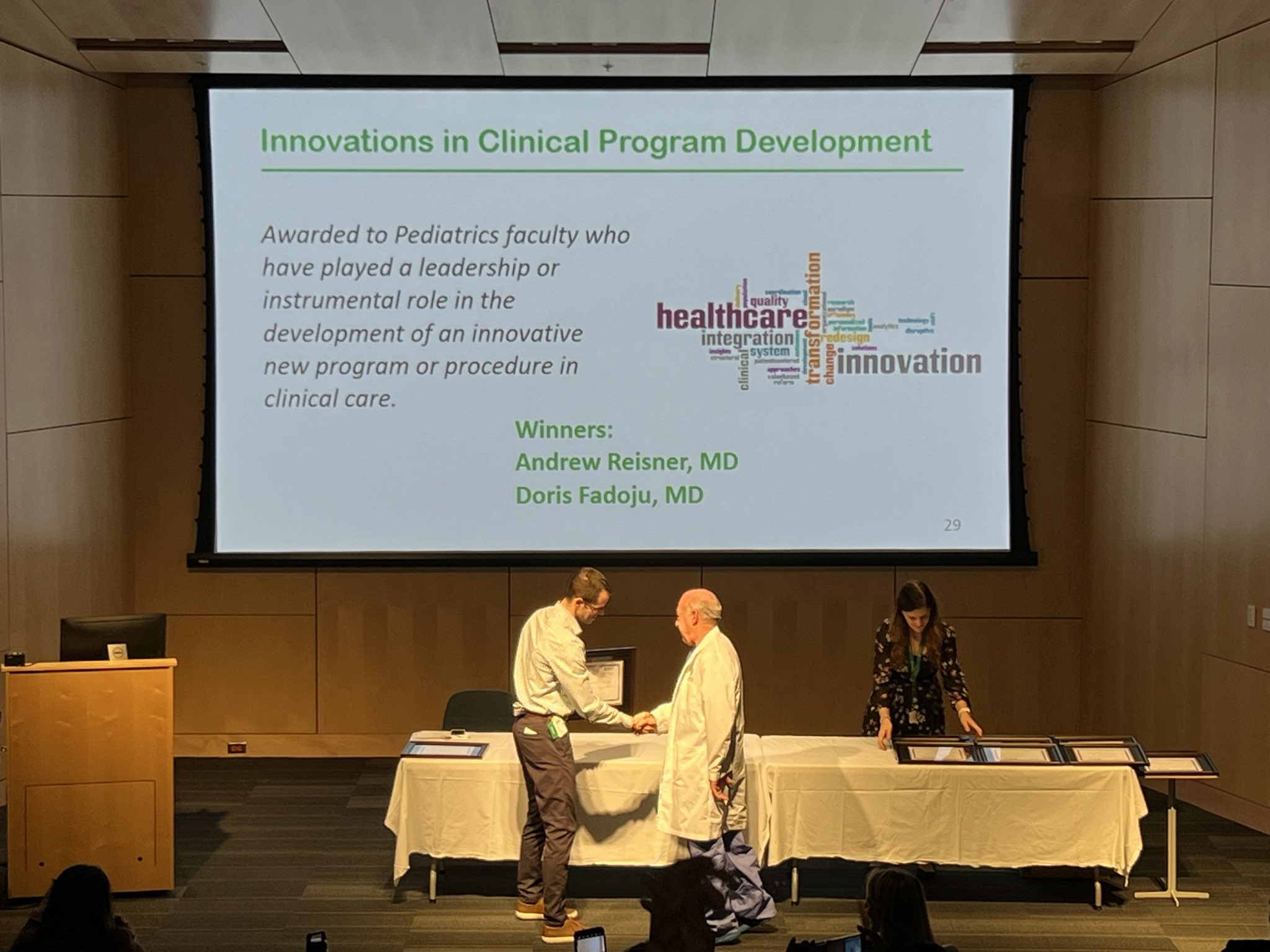
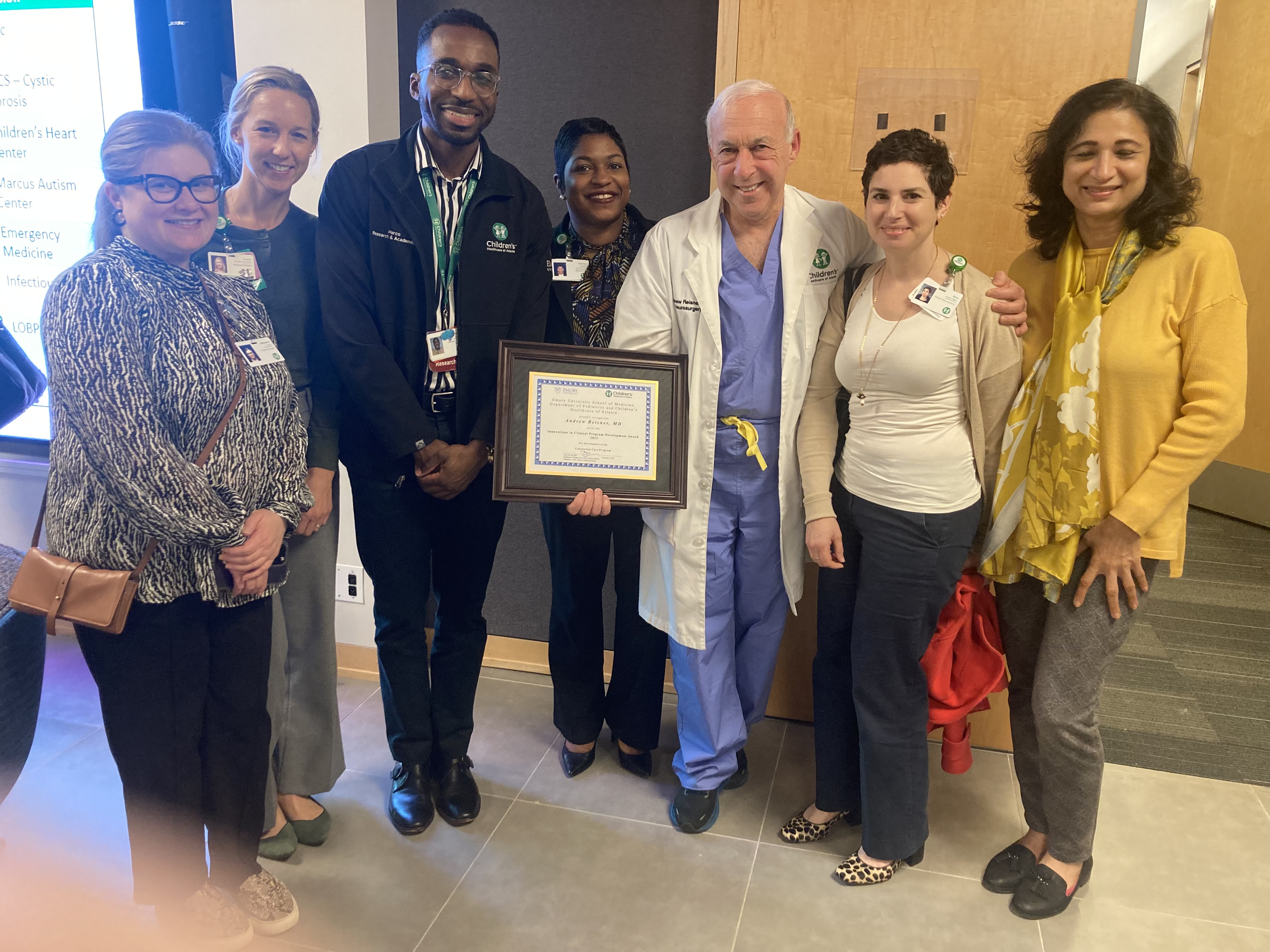
Dr. Reisner was awarded "Innovations in Clinical Program Development Award 2023" at Emory Department of Pediatrics and Children's Healthcare of Atlanta's 2023 Pediatrics Physician, Faculty & Staff Awards Celebration! He was awarded for his development of the Concussion Care Program. Congratulations Dr. Reisner!

Also in November, Dr. Reisner attended the Centenial Anniversary of the Serbian Neurosurgery Society Meeting, Belgrade, Serbia!
Dr. Reisner was honored as 1 of 7 international guests who were made honorary Serbian Neurosurgery Society members during the 100th annual Serbian Neurosurgery Meeting.

In addition, Dr. Reisner presented on Post-traumatic Aneurysms.
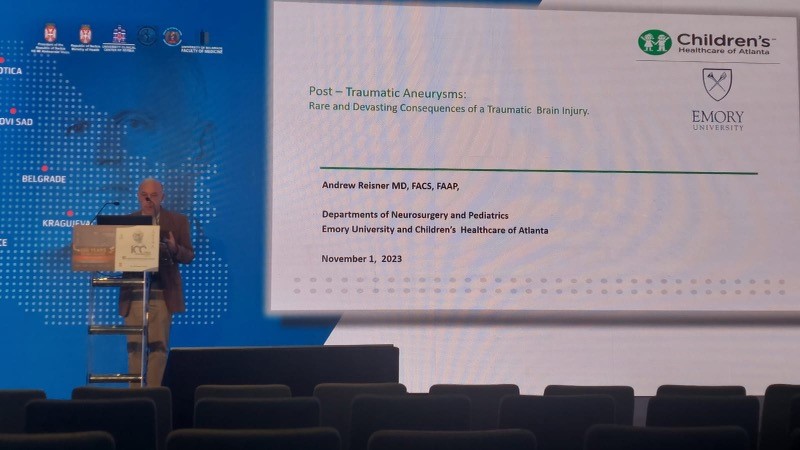
He also moderated a session on Neurotrauma with Professor Tariq Khan.

September 2023:
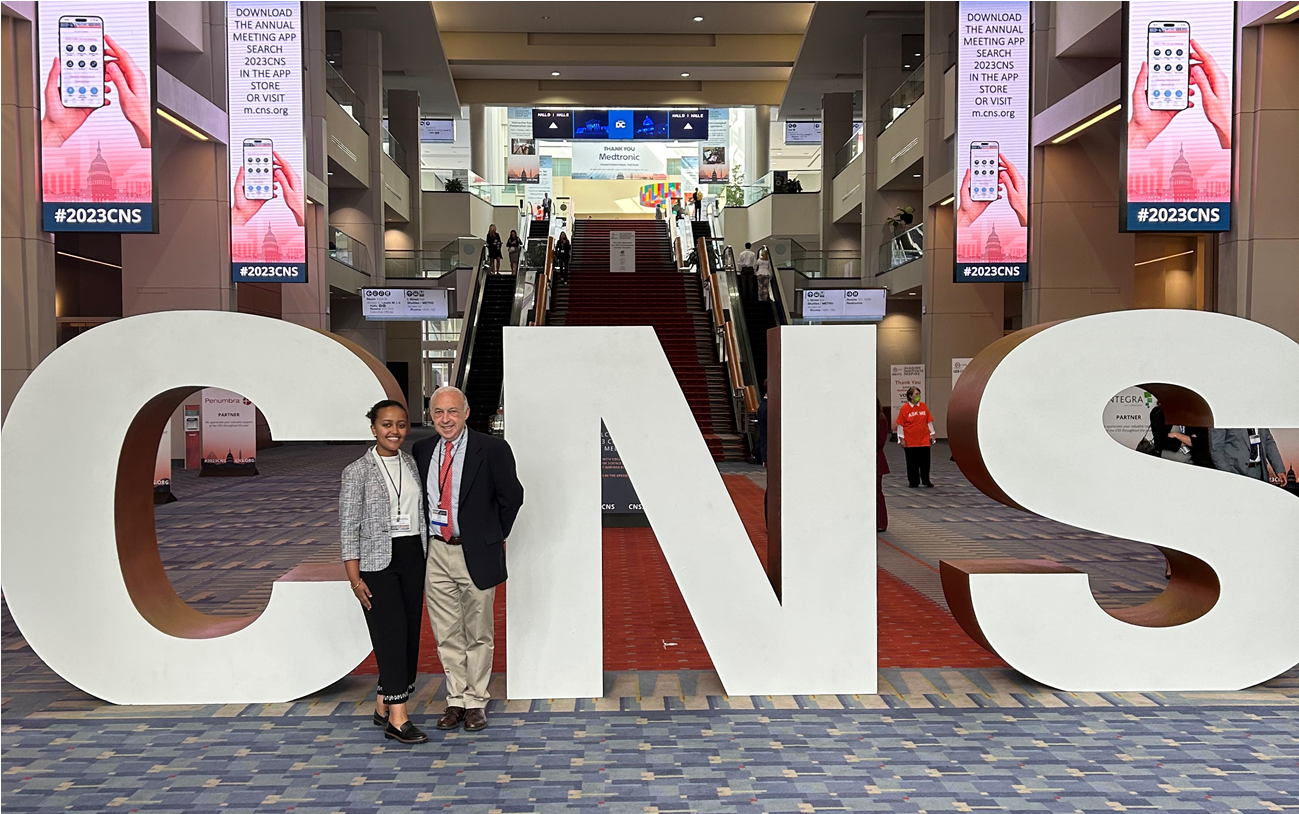
Dr. Reisner and Research Assistant Makda Mulugeta attended the Congress of Neurological Surgeons 2023 Annual Meeting, Washington, D.C.
Mulugeta, M, Reisner, A, et al. presented Emerging Risk Factor in Pediatric Intracranial Gunshot Wounds: Age under 5 years, which was awarded Top 3 Posters in Disparities in Healthcare.
July 2023:
Dr. Blackwell, Dr. Reisner, Senior Research Coordinator Meena Verma, Research Assistants Gabrielle Bailey and Makda Mulugeta, and student Kendall Parsons attened the National Neuotrauma Conference 2023 in Austin, TX!

Bailey, G, et al. presented on Social Determinants of Health as Predictors of Pediatric Concussion Outcomes (poster & oral presentation) and was awarded Top 20 Trainee Posters and Trainee Diversity Award.
Makda Mulugeta, et al. presented on Applying Known Prognostic Factors of Mortality in Pediatric Intracranial Gunshot Wounds to a Younger Cohort.
 \
\
Kendall Parsons, et al. presented on Socioeconomic Health Disparities in Pediatric Traumatic Brain Injury: Comparisons of Hispanic and Non-Hispanic Children.

June 2023:
PNL attended the Southeastern Pediatric Research Conference, Atlanta, GA!
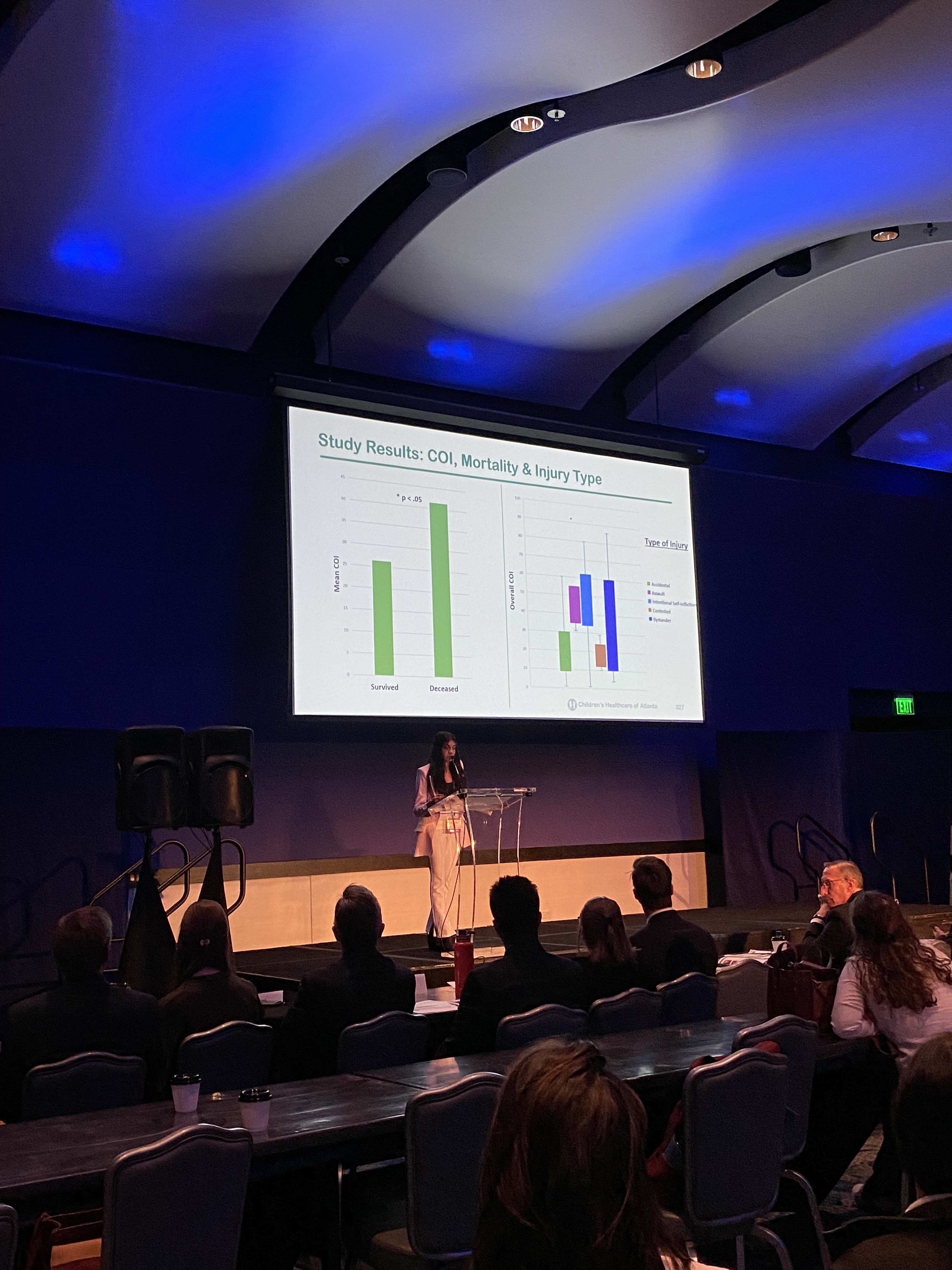
Image 1: Ruhika Aguru, et al. Relationship Between Child Opportunity Index and Mortality in Pediatric Patients with Intracranial Firearm Injuries (oral presentation)
Image 2: Makda Mulugeta & Gabrielle Bailey, et al. Trends in Pediatric Gunshot Wound Cases During the COVID-19 Pandemic.
April 2023:
Dr. Reisner Presenting at ICRAN 2023 in Santa Cruz, Bolivia.
CLICK TO WATCH : ICRAN 2023 SUMMARY VIDEO


January 2023:
The PNL Lab is now participating in the GEO-TBI study, "an international, prospective observational study on traumatic brain injury epidemiology". Read more about it here.
December 2022:
Dr. Reisner Presents at the 2022 Mediterranean Association of Neurological Surgeons: Cairo, Egypt Dec. 2022
.jpg)

PATIENT STORIES & HIGHLIGHTS:
To receive PNL's CV, please email PediatricNeurotraumaLab@choa.org
To view Dr. Reisner's CV, CLICK HERE.